
| Home |
| News 04/03/2544 |
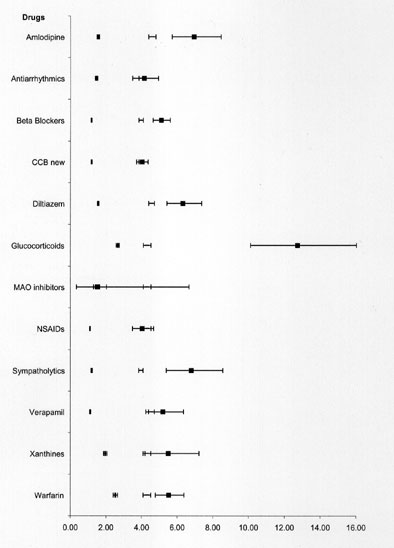
| From Medscape Pharmacists Drug Use Contraindications and Precautions in Congestive Heart Failure Robert A. Hamilton, PharmD |
| Novartis Claims Lead in Race to Find Novel COPD Therapies |
Rosiglitazone Twice Daily Improves Glycemic Control More Than Once-a-Day Dosing |
| Consumer Group Urges FDA Probe into Schering-Plough Manufacturing Practices |