
| Home |
| Pharmacy Cardiovascular Council Treatment Guidelines for the Management of Type 2 Diabetes Mellitus: Toward Better Patient Outcomes and New Roles for Pharmacists David Hawkins, Pharm.D., J. Chris Bradberry, Pharm.D., Mark J. Cziraky, Pharm.D., Robert L. Talbert, Pharm.D., David W. Bartels, Pharm.D., and Joli D. Cerveny, Pharm.D. Pharmacotherapy 22(4):436-444, 2002. © 2002 Pharmacotherapy Publications |
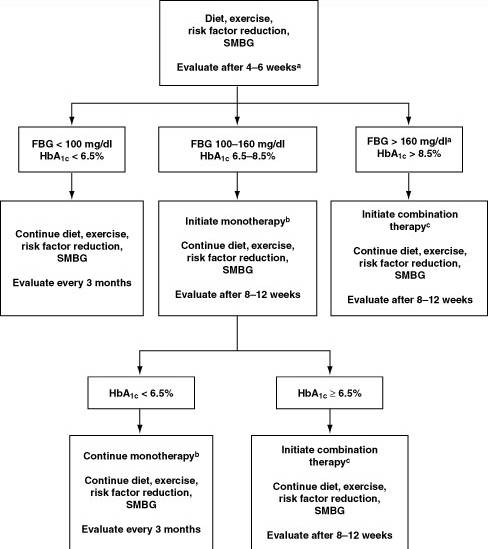
Figure 1. National Pharmacy Cardiovascular Council guideline for the treatment of type 2 diabetes mellitus. SMBG = self-monitoring of blood glucose concentration; FBG = fasting blood glucose (to convert to FPG values, add 10 mg/dl); HbA1c = hemoglobin A1c. a, Short-term insulin therapy to reduce glucose toxicity may be indicated in patients with FBG concentrations > 300 mg/dl. b, Monotherapy options are sulfonylurea, repaglinide or nateglinide, metformin, or glitazones. Therapy with an insulin sensitizer (metformin or glitazone) is recommended. c, Combination therapy options include oral and insulin combinations (oral + oral; oral + insulin). Inclusion of an insulin sensitizer is recommended.
Biochemical Index Normal
ValueDiagnostic
CriteriaHemoglobin A1c (%) < 6 NA Fasting plasma glucose (mg/dl) < 110 >/= 126 Plasma glucose 2 hrs after a 75-g oral glucose tolerance test (mg/dl) < 140 >/= 200
NA = not an acceptable instrument for diagnosing diabetes.
Mechanism of Action Metformin (immediate or extended release) Decreased insulin resistance, decreased hepatic glucose output, increased peripheral glucose utilization Sulfonylureas, meglitinides, nateglinide Increased insulin secretion a-Glucosidase inhibitors Delayed digestion of complex carbohydrates Glitazones Decreased insulin resistance, decreased hepatic glucose output, increased peripheral glucose utilization
Sulfonylurea Meglitinide Metformin Glitazone a-Glucosidase
InhibitorInsulin Sulfonylurea - - + + + + Meglitinide - - + + + + Metformin + + - + + + Glitazone + + + - + +a a-Glucosidase inhibitor + + + + - + Insulin + + + +a + -
+ = effective combination; - = inappropriate combination.
a Pioglitazone only.